LYMPHEDEMA - What You Haven't Been Told and Need to Know
What is Lymphedema
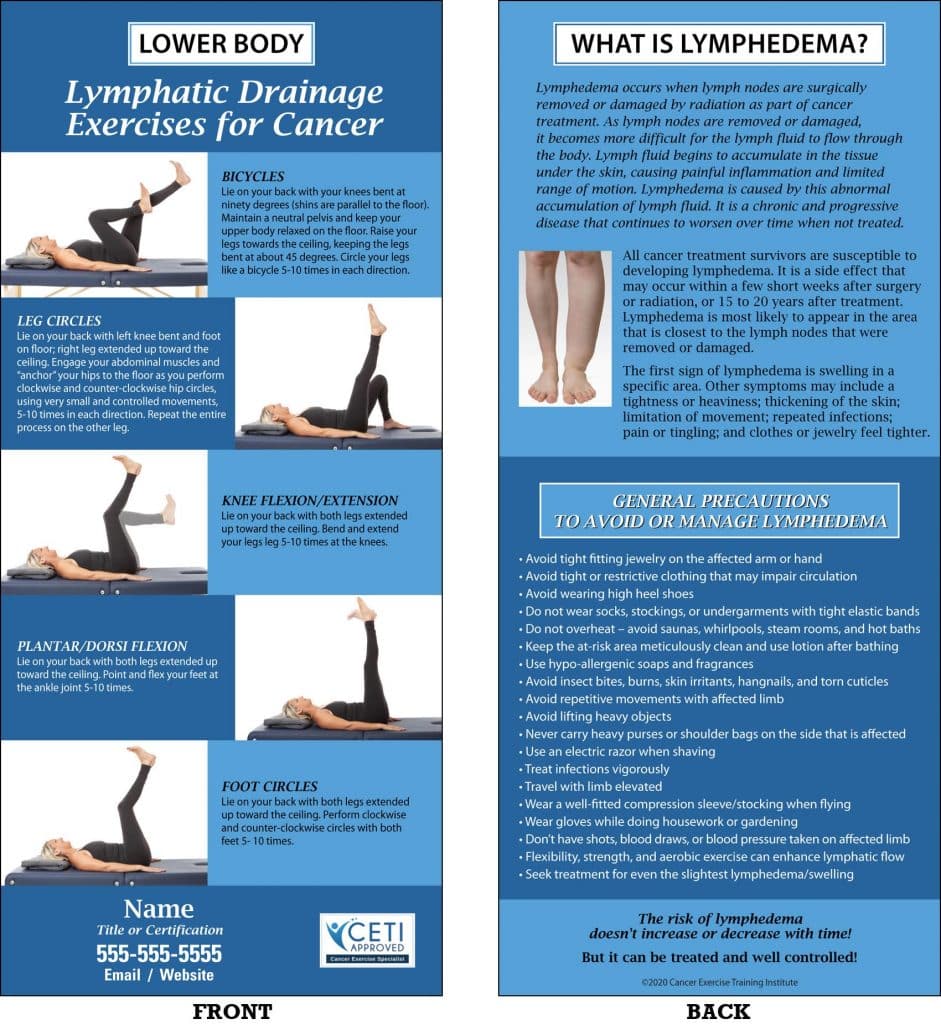
Lymphedema is swelling produced by an accumulation of lymph fluid in the tissue. Removal of the nodes and damage to the area prevents the lymph fluid in the area from draining properly, allowing it to accumulate in the tissue by restricting pathways and causing a back-up. It has been well documented that the development of lymphedema after cancer surgery and radiotherapy is related to the extent of the lymph node dissection, the extent of the surgery, and whether radiotherapy is given to the affected area. If lymphedema goes untreated, it can result in decreased limb function and range of motion, and numbness in the feet and toes. In addition, this damage may result in pain and tightness in the area as the lymph vessels close up, tighten, and sometimes snap. In lower extremity and torso cancer patients, the swelling can occur in the abdomen, pelvis, and in either leg/foot due to damage to the lymph vessels in the area caused by the removal of lymph nodes or from radiation to that area. The job of the lymphatic vessels is to drain fluid from the tissue cells in the body, along with protein molecules, bacteria, cellular waste products, and other unusable matter. This protein-rich fluid, called lymph once it is in the lymphatic system, travels in one direction: toward the heart. It is transported through the lymphatic vessels to the lymph nodes, where it is filtered and cleansed before returning to the venous system and moving on to the heart. In the heart, the fluid is simply returned to the blood to be recirculated by the body.

Who is at Risk for Lower Extremity Lymphedema?
If the lymphatic system has been injured, as in the case of a lymph node dissection or radiotherapy, the lymph can become backed up. If untreated, the backed-up fluid can provide a breeding ground for bacteria that can result in infection and can delay wound healing. A long-term accumulation of this fluid eventually results in thick and hardened tissues (fibrosis), which creates further resistance to draining the fluid from the limb. While lymphedema may not occur immediately after surgery, it can occur at any time during the rest of your life after cancer treatment. Sometimes extensive trauma can be the contributing factor while at other times it may be due to a bug bite, cat scratch, or burn. Radiotherapy also increases the chance of developing lymphedema. Radiotherapy is generally recommended to patients with a high risk of recurrence of cancer, such as those who have large, aggressive tumors. It is also recommended for those whose lymph nodes test positive for cancer cells or show an incidence of microscopic residual disease after surgery. Because lymph nodes are radiosensitive, radiotherapy depletes the lymphocytes in the nodes and decreases their filtering function and immune function.
Lymphedema can only affect the area where the nodes have been irradiated, not the overall immune system. After radiotherapy, the nodes become scarred and fibrotic, increasing the potential for blockage. With proper education and care lymphedema can be avoided or, if it develops, kept well under control. Older individuals and those with poor nutrition face an increased risk; as do individuals with infections.
What are the Stages of Lymphedema?
Guarding against infection is extremely important because the affected area will be more susceptible to infection and infection can cause increased swelling. If you notice any signs of infection contact your doctor immediately. These signs include swelling, fever, or skin that is red, tender, warm, persistently itchy or blotchy. There are four categories for grading lymphedema; grade one – four. Grade one is considered the latent or pre-clinical stage; it simply means that you are at risk for developing lymphedema, but there are no current signs or symptoms. In grade two, when the skin is pressed the pressure will leave a pit that takes some time to fill back in. This is referred to as pitting edema. Sometimes the swelling can be reduced by elevating the limb for a few hours. There is little or no fibrosis at this stage, so it is usually reversible. In grade three, when the swollen area is pressed, it does not pit and the swelling is not reduced very much by elevation. If left untreated the tissue of the limb gradually hardens and becomes fibrotic. In grade three the lymphedema is often referred to as elephantiasis. It occurs almost exclusively in the legs after progressive, long-term, and untreated lymphedema. At this stage there may be gross changes to the skin. There may even be some leakage of fluid through the tissue in the affected area, especially if there is a cut or sore. While lymphedema will respond to treatment, at this stage it is rarely reversible.
Lymphedema is a very serious condition and should not be taken lightly. It frequently results in complications, such as lymphangitis (a bacterial infection of the lymphatic system), skin changes, fibrosis, and infection. There are even a few life-threatening complications. Although rare, the development of a rare type of cancer, lymphangiosarcoma, is possible in the affected area. This can occur in patients with long-term, untreated, or improperly treated lymphedema. Unfortunately, this condition requires immediate amputation. Lymphedema may worsen with time if it is not attended to. It can become disabling by stiffening the joints or making the limbs heavy, and may cause significant cosmetic deformities.
What are Compression Garments?
Compression garments and bandages apply external pressure to a swollen limb. When swelling has persisted in an area, the tissue loses some of its elasticity and does not return to its’ original position and shape, even when the fluid decreases. The bandages support the skin and underlying blood vessels. The number of bandages used depends on the size of the limb and how effectively the compression is achieved. Many therapists recommend wearing the bandages while sleeping, as well as anytime that you are engaging in physical activity or exercising. In addition to bandaging, most patients should be fitted with a compression garment(s) that is worn during the daytime. The garments are not designed to reduce swelling, however, but to maintain the size of the limb and prevent swelling from increasing. Some patients will use compression stockings when flying on an airplane in order to reduce their chances of getting lymphedema due to changes in cabin pressure.
What Do I Need to Know About Air Travel?
When you are traveling by airplane, it is important to wear fitted stockings due to pressure changes which allow fluid to pool in the extremities. Due to the lack of movement during flight, the vessels which normally pump the lymph towards the regional lymph nodes are working at a very low level. Therefore, it is not only important to wear compression garments, but to move around the cabin whenever possible to prevent the pooling that can increase lymphatic load. While each of these precautions, as well as those listed on the following pages, make perfect sense, there are several other factors that can also influence a potential lymphedema outcome. These include, but are not limited to, the number of lymph nodes that were removed from a given location, the extent of surgical disruption, the amount of lymphatic scarring from radiation, and the degree of obesity.
Exercise and Lymphedema
One of the most important and often over looked components of exercise is breathing. Not only does breathing allow precious oxygen to be circulated through the bloodstream, but it is also effective for moving fluid through a gentle pumping action of the abdominal muscles. The fluid is pumped through the central lymphatic vessel in the chest cavity, stimulating the flow of lymph. When you breathe in using your abdominal muscles, the pressure in the chest cavity changes, because the belly breath moves your diaphragm. When you exhale, the pressure changes once again. This back-and-forth alternation in the pressure acts like a pump on the large lymphatic trunk that runs up through the chest cavity and drains into the venous system of the neck.
Here’s how; sit in an upright position. Take a deep breath through your nose and exhale through your mouth, flattening your belly and squeezing out every last bit of air. Emptying the lungs completely and removing all of the stale air from the bottom of the lungs automatically stimulates a diaphragmatic breath. Breathe in through your nose and notice how your belly expands. Repeat the sequence again. Let the air out through your mouth, making sure your belly flattens. Try another one or two breaths this way. If you get light-headed, try to slow down your inhalation, and pause before breathing in again. It is not necessary to breath with a giant breath – just one that goes to the bottom of your lungs, while your chest remains still. Imagine a balloon in your stomach that inflates when you inhale and deflates when you exhale.
Everyone knows the benefits of exercise for seemingly healthy individuals, but they carry even more a punch for those suffering from lymphedema. Generally speaking, those who exercise have a lower percentage of body fat. Keeping body fat in check can actually help to prevent lymphedema. Fat can be a special problem with an impaired lymphatic system. Fat is deposited in the interstitial tissue and can make it more difficult for the fluid to pass through and into the lymph vessels. The lymphatic system is stimulated by the pumping action of the blood vessels, as well as the pumping action of muscles, so anything one does to improve their circulatory system will be helpful for the lymphatic system.
A good exercise goal, for aerobic activity, is thirty minutes five times per week. Choose an exercise that will allow you to mildly increase your heart rate without “over-doing” it. It is important that you wear your support garment (if one has been prescribed for you) or bandage while exercising. Bandages increase pressure against the skin during exercise. The pressure, coupled with the contraction of your muscles, encourages the lymph to move. Exercise, in and of itself, will help to pump the muscles, improve circulation, and move lymph from congested areas into an area where it can drain more efficiently. It is important to start out very slowly with few repetitions and wait until the next day to see how the affected limb has responded. You can gradually increase your repetitions, based on what the limb will tolerate. Take your time and use good form and posture.
Warning Signs to Stop Exercising
When you have a fever.
• If you experience chest pain.
• If you experience sudden shortness of breath or unusual fatigue.
• If you have recurring leg pain or cramps.
• If you experience an acute onset of nausea during exercise.
• If you feel disoriented or confused.
• If you have had recent bone, back, or neck pain that is not relieved with rest.
• If you have an irregular heartbeat.
Precautions to Avoid Lower Extremity Lymphedema
• Avoid insect bites, burns, and skin irritants on the affected area
• Wear loose fitting clothing on torso and legs
• Don’t overheat – avoid saunas, whirlpools, steam rooms, hot baths, and sun bathing.
• If you are overweight and have experienced swelling, losing weight can help reduce it by reducing the amount of fatty tissue which retains fluid and blocks lymphatic pathways.
• Remember exercises with repetitive lower-body movements may increase your risk
• Avoid heavy lifting with the affected area; when you begin to exercise slowly and gradually add repetitions and resistance to see what your body and lymphatic system will tolerate
• When traveling by air, patients with lymphedema, or those who are at risk, must wear well-fitted compression stockings
• Use an electric razor when shaving legs
About the author:
Andrea was the PFP/Club Industry 2019 Personal Trainer of the Year. Since 1992 Andrea has been certified as a Corrective Exercise Specialist and Performance Enhancement Specialist by The National Academy of Sports Medicine (NASM), as a Personal Trainer by The American College of Sports Medicine (ACSM), the National Academy of Sports Medicine (NASM), and the American Council on Exercise (ACE), as a Special Populations Expert by The Cooper Institute. Andrea will complete her Master’s in Functional Nutrition in the summer of 2023.
Andrea is a subject matter expert for Medical Wellness Association, chairperson for the Medical Fitness Foundation Education Advisory Board and on the advisory board for the MedFit Network .
Andrea is a 39-year cancer survivor and has/had 23 first-degree relatives diagnosed with cancer. In 2015 she lost her father, Morton, to complications of bladder cancer and prostate cancer, and myelodysplastic syndrome. Her mother is currently fighting stage 4 metastatic breast cancer after a 23-year remission.
At the age of eighteen, Andrea was diagnosed with thyroid cancer and underwent a complete thyroidectomy and radioactive iodine treatment. Following her surgery, Andrea was challenged with a new, sluggish metabolism, and weight gain. It was through her own personal struggles to regain her previous energy level and physique that Andrea decided to become a personal trainer. She wanted to be able to help others, like herself, who struggled with the same issues of weight gain and poor self-esteem. Andrea graduated from the University of MD in 1990 with a degree in Criminal Justice, but quickly realized that she was in the wrong profession. She avidly pursued a career as a personal trainer.
Andrea began training in 1992 and worked at the National Capital YMCA in Washington, D.C. She quickly worked her way up to Director of Personal Training and ran the department for several years. While working at the YMCA, Andrea started Leading Edge Fitness and EMPOWER- Energizing, Mobilizing, Post-Operative Workout Enhancing Recovery. In 1996 Andrea’s mom was diagnosed for the second time with breast cancer. She watched her mother struggle through the trauma of multiple surgeries, reconstruction, a frozen shoulder, and addiction to narcotics in order to cope with the pain associated with her surgeries.
Inspired by her mother, Andrea, along with a medical advisory board from Georgetown University, George Washington University, and Johns’ Hopkins University Medical Centers, set out to write “Essential Exercises for Breast Cancer Survivors.” The goal was to help the millions of men and women, like her mother, to gain back their strength, range of motion, and self-esteem (among other things), following breast cancer surgery and treatment. The book was published by Harvard Common Press in 2000. Shortly thereafter, Andrea founded The Breast Cancer Survivor’s Foundation, a 501c3 public charity—to better the lives of cancer survivors and their families.
Realizing that she is limited to helping a certain number of clients per week, Andrea founded The Cancer Exercise Training Institute in 2004 and developed the Cancer Exercise Specialist® and Breast Cancer Recovery BOSU® Specialist™ Advanced Qualifications for health and fitness professionals. Through this program she has been able to pass on her wealth of knowledge, and enable health and fitness professionals around the world, to work safely and confidently with cancer patients. Through CETI’s Advanced Qualification live workshops and home study, participants learn about twenty-six types of cancer and pediatrics, their surgeries, treatments, lymphedema identification, prevention, and treatment, reconstructive procedures, contraindications, side-effects and so much more. Following a comprehensive examination, attendees are awarded the Cancer Exercise Specialist® and/or Breast Cancer Recovery BOSU® Specialist ™Advanced Qualifications.
Andrea has presented the Cancer Exercise Specialist Workshop around the world and has been a guest speaker at IDEA World, Healthy Aging Summit, Asia Fitness Conference, CPTN Personal Training Conference, IRHSA, TSI Summit, Medical Fitness Tour, Kaiser Permanente Thriving with Cancer Conference, Winona State University – Survivors Unite, McHenry Community College, New York Institute of Technology, OHSU School of Nursing, Edwards Hospital, Georgetown University Hospital, Suburban/Johns’ Hopkins, Mennonite Cancer Foundation, South Georgia Medical Center, Cary Medical Center Lynchburg General Hospital, Chesapeake Regional Medical Center, Sibley Hospital, Memorial Hermann, Sandford Health System, Avera McKennan Prairie Cancer Center, Baptist Hospital East, Patricia Neal Rehab. Center, St. Mary’s, Baptist Health System, Southeast Georgia Cancer Coalition, and Fort Bliss Army Installation.

The Cancer Exercise Training Institute is considered the gold-standard of education in oncology exercise and has trained more individuals than any other organization in the world
If you would like to speak to Andrea about an individualized cancer recovery program that includes lymphedema education and prevention, correcting muscle imbalances and improving range of motion, regaining strength, losing body fat, and enhancing your overall wellness to reduce your risk for second cancers and co-morbidities like diabetes, osteoporosis, heart and lung disease, contact her through the link below.
